Tremor stability index: a new tool for differential diagnosis in tremor syndromes.
It can be a challenge to tell apart the two most common causes of shaking or ‘tremor’ in movement disorders, namely Essential Tremor and Parkinson’s disease tremor. Here, we describe our development of an accurate diagnostic aid that stems from brief, simple and cheap recordings of tremor in people. This new tool can be used to guide clinicians in selecting the correct diagnosis and treatment.
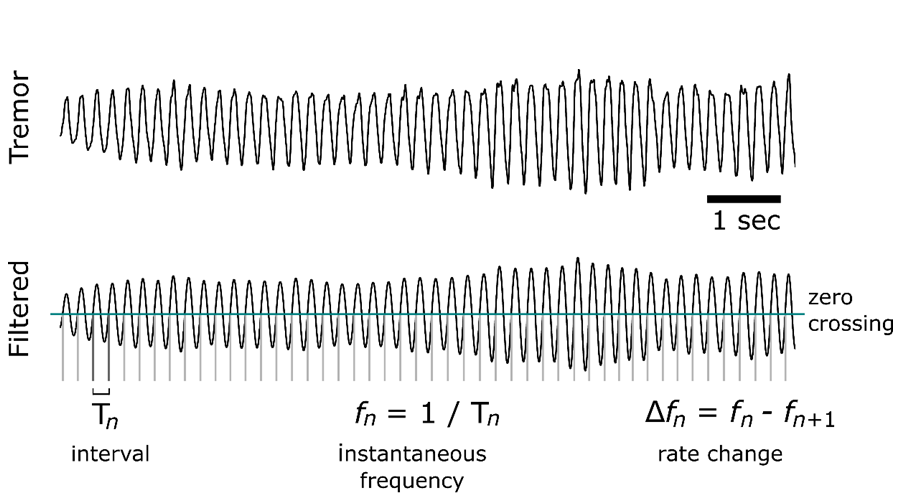
See Vidailhet et al. (doi:10.1093/brain/awx140) for a scientific commentary on this article.Misdiagnosis among tremor syndromes is common, and can impact on both clinical care and research. To date no validated neurophysiological technique is available that has proven to have good classification performance, and the diagnostic gold standard is the clinical evaluation made by a movement disorders expert. We present a robust new neurophysiological measure, the tremor stability index, which can discriminate Parkinson's disease tremor and essential tremor with high diagnostic accuracy. The tremor stability index is derived from kinematic measurements of tremulous activity. It was assessed in a test cohort comprising 16 rest tremor recordings in tremor-dominant Parkinson's disease and 20 postural tremor recordings in essential tremor, and validated on a second, independent cohort comprising a further 55 tremulous Parkinson's disease and essential tremor recordings. Clinical diagnosis was used as gold standard. One hundred seconds of tremor recording were selected for analysis in each patient. The classification accuracy of the new index was assessed by binary logistic regression and by receiver operating characteristic analysis. The diagnostic performance was examined by calculating the sensitivity, specificity, accuracy, likelihood ratio positive, likelihood ratio negative, area under the receiver operating characteristic curve, and by cross-validation. Tremor stability index with a cut-off of 1.05 gave good classification performance for Parkinson's disease tremor and essential tremor, in both test and validation datasets. Tremor stability index maximum sensitivity, specificity and accuracy were 95%, 95% and 92%, respectively. Receiver operating characteristic analysis showed an area under the curve of 0.916 (95% confidence interval 0.797-1.000) for the test dataset and a value of 0.855 (95% confidence interval 0.754-0.957) for the validation dataset. Classification accuracy proved independent of recording device and posture. The tremor stability index can aid in the differential diagnosis of the two most common tremor types. It has a high diagnostic accuracy, can be derived from short, cheap, widely available and non-invasive tremor recordings, and is independent of operator or postural context in its interpretation.