Acute effects of adaptive Deep Brain Stimulation in Parkinson's disease.
Adaptive deep brain stimulation (aDBS) holds promise for treating movement difficulties in Parkinson’s. Previous trials of aDBS have taken place immediately after electrodes were implanted. Here, we trial this therapeutic approach in patients whose electrodes were implanted years before. The same benefits of aDBS were seen under these conditions, which are more representative of the chronic treatment state.
Background: Beta-based adaptive Deep Brain Stimulation (aDBS) is effective in Parkinson’s disease (PD), when assessed in the immediate post-implantation phase. However, the potential benefits of aDBS in patients with electrodes chronically implanted, in whom changes due to the microlesion effect have disappeared, are yet to be assessed.
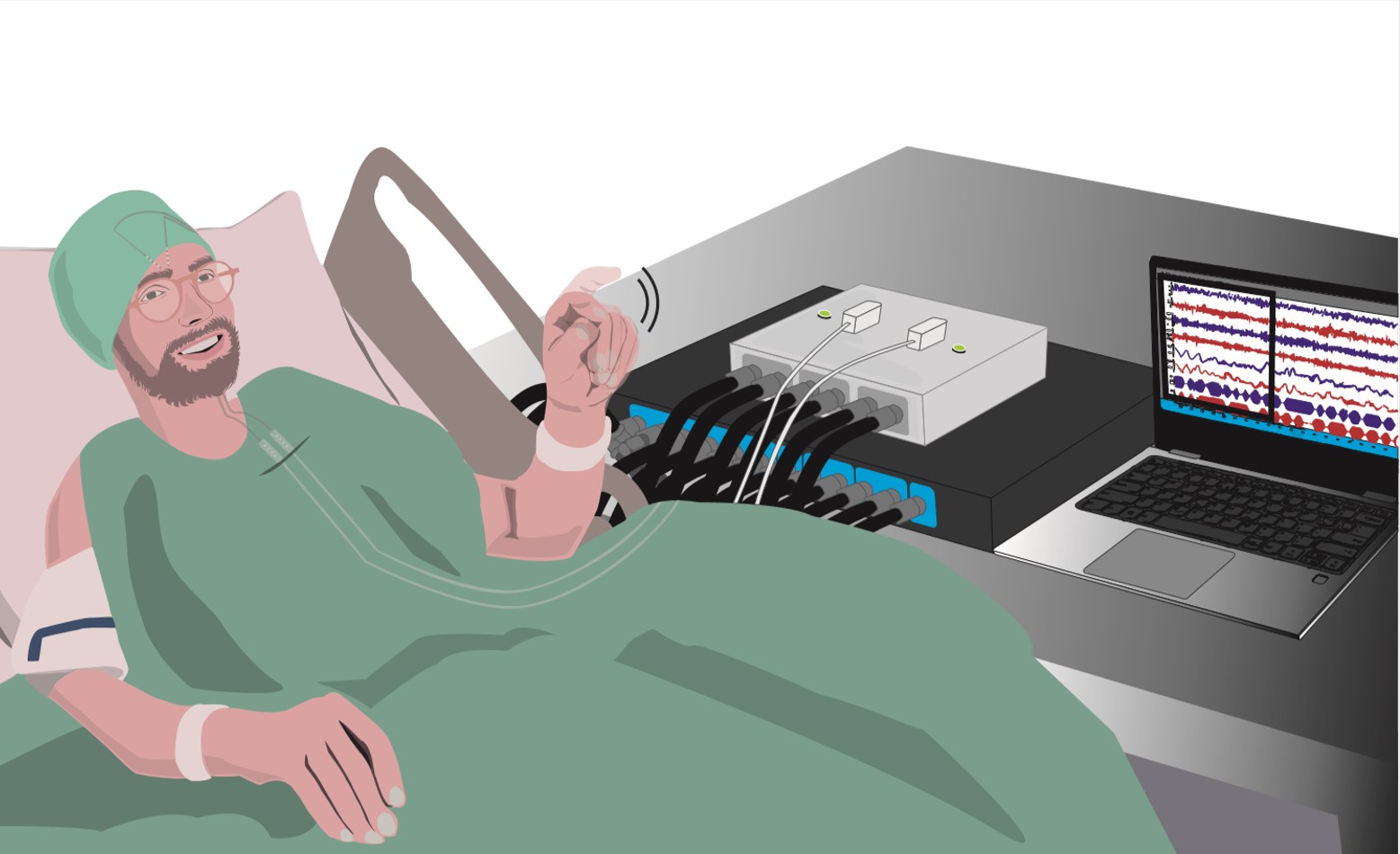
Methods: To determine the acute effectiveness and side-effect profile of aDBS in PD compared to conventional continuous DBS (cDBS) and no stimulation (NoStim), years after DBS implantation, 13 PD patients undergoing battery replacement were pseudo-randomised in a crossover fashion, into three conditions (NoStim, aDBS or cDBS), with a 2-min interval between them. Patient videos were blindly evaluated using a short version of the Unified Parkinson’s Disease Rating Scale (subUPDRS), and the Speech Intelligibility Test (SIT).
Results: Mean disease duration was 16 years, and the mean time since DBS-implantation was 6.9 years. subUPDRS scores (11 patients tested) were significantly lower both in aDBS (p= <0.001), and cDBS (p = 0.001), when compared to NoStim. Bradykinesia subscores were significantly lower in aDBS (p = 0.002), and did not achieve significance during cDBS (p = 0.08), when compared to NoStim. Two patients demonstrated re-emerging tremor during aDBS. SIT scores of patients who presented stimulation-induced dysarthria significantly worsened in cDBS (p = 0.009), but not in aDBS (p = 0.407), when compared to NoStim. Overall, stimulation was applied 48.8% of the time during aDBS.
Conclusion: Beta-based aDBS is effective in PD patients with bradykinetic phenotypes, delivers less stimulation than cDBS, and potentially has a more favourable speech side-effect profile. Patients with prominent tremor may require a modified adaptive strategy.
2023. Brain, 146(12):5015-5030.
2022. NPJ Parkinsons Dis, 8(1):88.