Cortical signatures of sleep are altered following effective deep brain stimulation for depression.
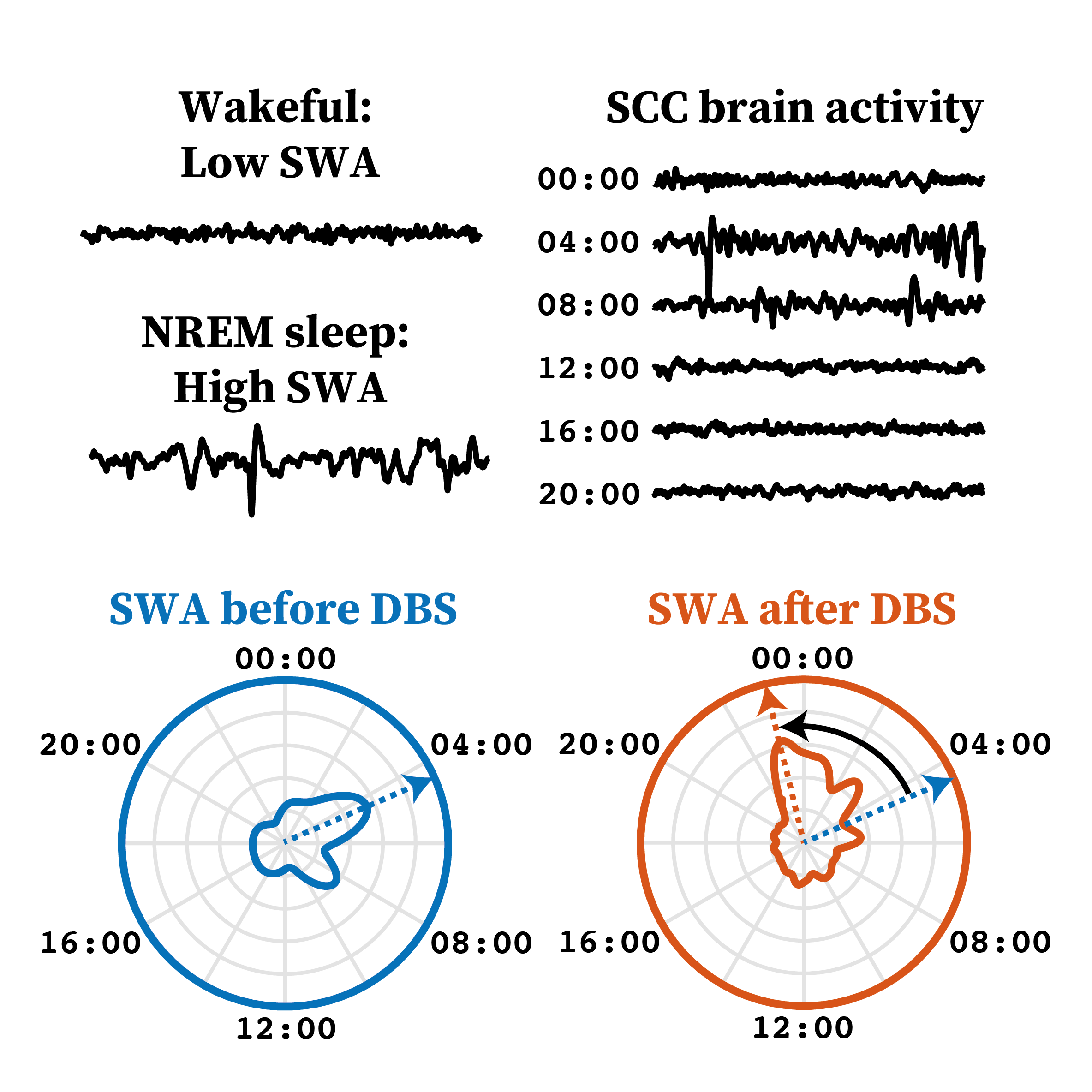
Depression is strongly linked with sleep quality. We used recordings from an implanted device providing a new brain stimulation therapy for depression to look at how sleep changed as patients got better. We found that they got more deep sleep earlier in the night, and showed increased ‘sleep spindles’ – brain waves with important cognitive functions. This could be an important part of how brain stimulation improves depression symptoms.
Deep brain stimulation (DBS) of the subcallosal cingulate cortex (SCC) is an experimental therapy for treatment-resistant depression (TRD). Chronic SCC DBS leads to long-term changes in the electrophysiological dynamics measured from local field potential (LFP) during wakefulness, but it is unclear how it impacts sleep-related brain activity. This is a crucial gap in knowledge, given the link between depression and sleep disturbances, and an emerging interest in the interaction between DBS, sleep, and circadian rhythms. We therefore sought to characterize changes in electrophysiological markers of sleep associated with DBS treatment for depression. We analyzed key electrophysiological signatures of sleep-slow-wave activity (SWA, 0.5-4.5 Hz) and sleep spindles-in LFPs recorded from the SCC of 9 patients who responded to DBS for TRD. This allowed us to compare the electrophysiological changes before and after 24 weeks of therapeutically effective SCC DBS. SWA power was highly correlated between hemispheres, consistent with a global sleep state. Furthermore, SWA occurred earlier in the night after chronic DBS and had a more prominent peak. While we found no evidence for changes to slow-wave power or stability, we found an increase in the density of sleep spindles. Our results represent a first-of-its-kind report on long-term electrophysiological markers of sleep recorded from the SCC in patients with TRD, and provides evidence of earlier NREM sleep and increased sleep spindle activity following clinically effective DBS treatment. Future work is needed to establish the causal relationship between long-term DBS and the neural mechanisms underlying sleep.
2024. Transl Psychiatry, 14(1):103.
2022. NPJ Parkinsons Dis, 8(1):88.
2023. Mov Disord, 38(5):818-830.
2022. Brain Stimul, 15(6):1513-1516.